William Check, PhD
September 2015—Emerging and re-emerging viruses are well and alive, says Sherif Zaki, MD, PhD, chief of the Infectious Diseases Pathology Branch, Centers for Disease Control and Prevention. At the Clinical Virology Symposium in April, he spoke on viral etiology in unexpected deaths, presenting a list of outbreaks of unexplained illnesses in which his branch took part in the past two decades and which turned out to be caused by viruses. It was hantavirus pulmonary syndrome in the U.S. in 1993, Nipah virus in Malaysia and Singapore in 1999, SARS worldwide in 2003, MERS in the Arabian Peninsula in 2012, and others since and in between. His focus at the symposium was transplant-associated viral infections.
“Pathologists are among the first to encounter infectious disease outbreaks and are in an excellent position to recognize them,” he told attendees. “Many examples of recent emerging infectious diseases have been diagnosed through autopsies, which are increasingly being viewed as effective surveillance tools.” This was well demonstrated by one transplant-related cluster that featured what Dr. Zaki called “the persistent pathologist.”
Culture, serology, electron microscopy, immunohistochemistry, and molecular techniques have been central to finding viral causes of disease outbreaks. “Our approach to these situations depends on the clinical and epidemiologic features of the outbreak combined with histopathology,” he said. “As pathologists, we recognize patterns of inflammation—acute, chronic, granulomatous—and if there is a cytopathic effect, we can see it.”
Transmission of unusual viral pathogens from a single donor to multiple recipients of transplanted organs is not an uncommon problem, and it’s a vexing one. “We are talking about donor-derived infections, which are unexpected, unrecognized at the time of death, and not screened for in the donor,” Dr. Zaki said. “Although there is a low incidence of such events, they are high profile.”
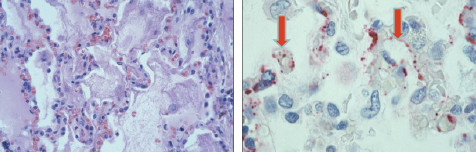
Hantavirus pulmonary syndrome. Photomicrographs of lungs: Pulmonary edema (left) and viral proteins (right). Courtesy Sherif Zaki, MD, PhD.
It is difficult to prevent these clusters for several reasons, he said: More than 25,000 transplants are done each year, 100,000 people are on waiting lists, availability of donor organs is limited, and there are few criteria for donor exclusion.
While transplant physicians have long been aware of the possibility of donor transmission of “typical” organisms, including cytomegalovirus, hepatitis B and C viruses, and Epstein-Barr virus, in the past 15 years several clusters owing to more unusual organisms have also occurred: microsporidia, lymphocytic choriomeningitis virus (LCMV), West Nile virus, and rabies. “These infections are unexpected and they attract a lot of public attention,” Dr. Zaki said, showing newspaper headlines calling into question the rules for organ transplantation.
He described investigations into clusters of transplant infections caused by lymphocytic choriomeningitis virus and rabies, highlighting the contributions of the pathologist and the laboratory.
In the first case a 51-year-old male organ recipient was found dead on the sidewalk with a subdural hematoma. Other recipients from the same donor also died. “We didn’t know the cause of death,” Dr. Zaki said. Serology for all the usual suspects was negative. It took six weeks to identify the virus as LCMV by culture, serology, histopathological examination with IHC staining, and electron microscopy. “In my opinion, these are very important tools for recognizing these diseases,” he noted.
In a second cluster, by contrast, which occurred a few years later, the patients had the same features as in the first, so investigators suspected LCMV from the outset. It took only a few days to identify the virus.
In the second case the donor was a mother who cleaned the cage of her daughter’s hamster; the cage was the source of LCMV infection. This finding underscores Dr. Zaki’s emphasis on the zoonotic nature of many clusters of unexpected illness.
Between the two LCMV incidents, seven of the eight recipients died. Both clusters were reported (Fischer SA, et al. New Engl J Med. 2006; 354:2235–2249).
“Since then we’ve had eight LCMV clusters,” Dr. Zaki said, “so something that we thought was uncommon is actually pretty common.” In one recent cluster, LCMV was identified by next-generation sequencing.
In a rabies cluster that occurred in 2004, the CDC was contacted by a pathologist in Texas about two deaths in transplant recipients and a third recipient with altered mental status, who also eventually died. The connection to a single donor came up in a fortuitous way: The patients’ families discovered it while talking in the ICU waiting room. The donor, who had a history of drug use, became ill and couldn’t swallow but was not diagnosed. The donor’s death was thought to be due to cocaine-induced brain hemorrhage.
“Our essential clue came from histopathology,” Dr. Zaki said. Staining on IHC showed Negri bodies in the brain, which are pathognomonic of rabies infection.
It is here that the “persistent pathologist” label arose. “The pathologist recalled another case of encephalitis,” Dr. Zaki said, “and went back and reviewed the autopsy.” It was consistent with encephalitis due to West Nile virus. The pathologist sent the slides to the CDC; staining showed rabies. However, this patient had received a liver from a different donor. “Was this nosocomial transmission?” Dr. Zaki asked. “Natural exposure? A second donor with rabies?”
Further investigation revealed that, while the liver came from a second donor, the artery stump to the liver came from the initial rabies-infected donor. If a surgeon doesn’t need a good artery from a donated organ, he or she may save it for another transplant, Dr. Zaki explained in a recent CAP TODAY interview. As a result, a transplant unit has “bits and pieces of tissue stored in a freezer.” In the case of the fourth rabies-infected recipient, the surgeon pulled from the freezer the artery stump from the infected donor and used it.
“A lot has changed in policies of tracking tissues and organs and it would be more difficult for this incident to happen now,” Dr. Zaki said. “They would know it was from the same donor, and if there was a problem all organs and tissues [from that donor] would be withdrawn.”
In a more recent case, a renal transplant recipient died 18 months after transplantation. “That is too long for rabies,” Dr. Zaki said. “I was betting this was not rabies.” However, Negri bodies were present in neurons of the brain, establishing the diagnosis. The donor also tested positive by PCR and histopathology. Further testing found it to be raccoon rabies, which Dr. Zaki said may explain the longer incubation period. He and his co-investigators recommended: “Rabies should be considered in patients with acute progressive encephalitis of unexplained etiology, especially for potential organ donors. A standard evaluation of potential donors who meet screening criteria for infectious encephalitis should be considered, and risks and benefits for recipients of organs from these donors should be evaluated” (Vora NM, et al. JAMA. 2013;310:398–407).
When Dr. Zaki was asked after his talk for advice on how to prevent clusters of transplant-derived infections with unusual viruses, he said, “When a person is at the door of death and they get an organ, it is hard to be picky.” Aside from routine testing for common infections and obtaining a donor exposure history, such as to pets and rodents, little can be done.
With regard to preventing transmission of lymphocytic choriomeningitis virus, Dr. Zaki tells CAP TODAY, “Unfortunately, we can’t really rely on screening donors. We can pick up some LCMV infections by serology and PCR, but most infected persons have such a low level of virus that we can’t detect it by laboratory testing.” Neither of the donors in the two clusters Dr. Zaki described tested positive for LCMV, even after that virus was identified in the recipients.
“As a pathologist, I push for the importance of donor autopsies,” Dr. Zaki said. “I feel very strongly about that. You are harvesting tissues and organs, so why not get the brain and other tissues that will allow you to test for infectious agents.” Even if a virus is found a week or two after transplantation, he noted, clinicians can be on the watch for it in the recipient. Then, too, prophylaxis, such as for rabies, may prevent illness.
To illustrate further the important part pathology plays in helping to uncover viral causes of outbreaks, Dr. Zaki presented pertinent aspects of several investigations. He begins with hantavirus pulmonary syndrome. Young people in the Four Corners region of the U.S., largely Native Americans, were dying of a flu-like illness with a high mortality rate—about 60 percent. Death, which occurred within a couple of days of onset, was caused by massive pleural effusions; on x-ray the pleural fluid showed up as a “whiteout.” “Basically they were drowning in their own secretions,” Dr. Zaki said.
Autopsy verified the presence of massive pleural effusion. “The main finding was massive amounts—six to seven liters—of pleural effusion fluid in the pleural cavity,” he said. Histopathology showed interstitial pneumonitis with fibrin and edema around alveoli. Copious amounts of immunoblasts in lymph nodes and circulating in the blood indicated an activated immune system.
“We hypothesized that the cause was plague or influenza,” Dr. Zaki said. The first clue that an unexpected pathogen was responsible came from a serology test in the special virology section at the CDC showing elevated IgG to hantavirus, suggesting that a hantavirus could be the culprit. “This finding was met with lots of skepticism,” he said, for two main reasons. First, only one strain of hantavirus was known in the Western Hemisphere, and it was not pathogenic. Second, known hantaviruses were associated with hemorrhagic disease of the kidneys, not pulmonary effusion. So hantavirus didn’t seem to fit the outbreak profile.
Proof that a hantavirus was the causative agent came from immunohistochemistry in Dr. Zaki’s laboratory and PCR in the laboratory of Stuart Nichol, PhD, chief of the CDC Viral Special Pathogens Branch. Histochemistry showed hantavirus antigens in the lungs of patients as well as the virus targeting the microcirculation in lung capillaries, causing pulmonary edema. Thus, the world learned about a new condition—hantavirus pulmonary syndrome. About two dozen strains of hantavirus are now known throughout the Western Hemisphere, many of them pathogenic.
Hantavirus deaths still occur in the U.S., he noted, citing a small outbreak in Yosemite National Park in 2012.
A second revealing outbreak investigation took place in Sarawak, Malaysia in 1997. Children ages five months to six years were dying of cardiogenic shock; EKG abnormalities were documented. Many had hand, foot, and mouth disease and many had symptoms of aseptic meningitis, leading investigators to suspect coxsackievirus myocarditis. Tissues from a dozen or so hearts were submitted to the CDC, but there was no evidence of myocarditis. “Our breakthrough came with one patient from whom we got a block from the heart and one from the CNS,” Dr. Zaki said. Review of the central nervous system tissue revealed “raging encephalitis.”
Subsequent IHC for enterovirus in brain tissue was positive, leading to identification of strain EV 71, the first time this variant had been documented to cause encephalitis. Pathogenesis was different from the initial premise. Physicians had thought that myocarditis was causing the heart problems. But the primary target was the CNS, leading to neurogenic pulmonary edema. “This shows that pathology can give clues to what is happening,” Dr. Zaki said.
 CAP TODAY Pathology/Laboratory Medicine/Laboratory Management
CAP TODAY Pathology/Laboratory Medicine/Laboratory Management
