Editor: Frederick L. Kiechle, MD, PhD
Submit your pathology-related question for reply by appropriate medical consultants. CAP TODAY will make every effort to answer all relevant questions. However, those questions that are not of general interest may not receive a reply. For your question to be considered, you must include your name and address; this information will be omitted if your question is published in CAP TODAY.
Q. Should phosphate analysis be added to the comprehensive metabolic panel, especially given the test’s usefulness in distinguishing various bone disorders?
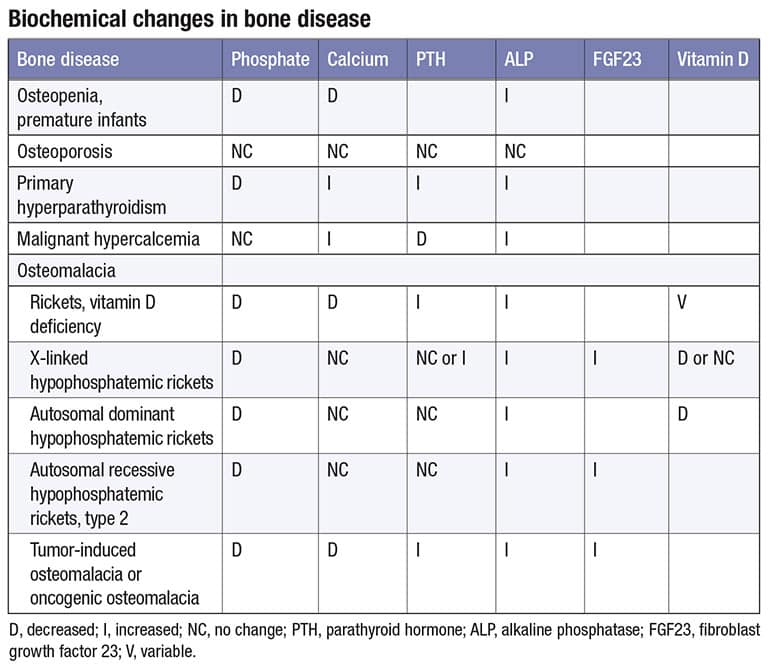
A.July 2023—Phosphate represents one percent of total body weight and has a normal reference range of 2.5 to 4.5 mg/dL. The reference range is highest in infants (4.5–8.3 mg/dL) and decreases with age. The majority of phosphate in the skeleton is in the form of hydroxyapatite crystals or amorphous calcium phosphate.1 There are two forms of phosphate in serum: dihydrogen phosphate (H2PO4) and monohydrogen phosphate (HPO4).1 The table illustrates biochemical changes in bone diseases.2,3,4Three hormones regulate phosphate homeostasis: vitamin D (calciferol) or D2 (ergocalciferol) and D3 (cholecalciferol), which are processed by the liver to 25-hydroxy vitamin D; parathyroid hormone; and fibroblast growth factor 23. FGF23 is produced by osteocytes or osteoblasts and consists of 251 amino acids with a signal peptide comprising 24 amino acids.3,5 It inhibits renal reabsorption of phosphate after binding to the FGFR1-Klotho complex.6 Alpha-Klotho serves as a co-receptor.6 Tumor-induced osteomalacia (TIO) is a rare paraneoplastic disorder caused by benign phosphaturic mesenchymal tumors that secrete FGF23 and can present anywhere in the body. TIO is diagnosed, on average, 2.9 years after the onset of symptoms, and the underlying tumor is identified, on average, 5.4 years after symptom onset. Therefore, a chronically low phosphate found via screening may be the only clue that points to the onset of TIO.2,3,5,6
Osteopenia is a condition in which bone mineral density is lower than the normal peak density but not low enough to be considered osteoporosis.4 Several diseases or therapies have been associated with increased bone fragility and fractures, including diabetes mellitus type 17 and type 2,8 hormone treatments for transgender transition (puberty blocks and gender-affirming therapy),9 and subclinical thyroid dysfunction with a thyrotropin level of less than 0.56 mIU/L.10
There are a variety of other disorders associated with hyperphosphatemia or hypophosphatemia that would benefit from a screening phosphate determination.11,12 It is clearly time to reassess whether to include serum phosphate in the comprehensive metabolic panel.
- Qadeer HA, Bashir K. Physiology, Phosphate. In: StatPearls. StatPearls Publishing; Aug. 2022. https://www.ncbi.nlm.nih.gov/books/NBK560925
- Lee J, Vasikaran S. Current recommendations for laboratory testing and use of bone turnover markers in management of osteoporosis. Ann Lab Med. 2012;32(2):105–112.
- Li L, Wang S-X, Wu M-W, et al. Acquired hypophosphatemic osteomalacia is easily misdiagnosed or neglected by rheumatologists: a report of 9 cases. Exp Ther Med. 2018;15(6):5389–5393.
- Elam REW. Osteoporosis. Medscape. Updated Dec. 21, 2022. https://emedicine.medscape.com/article/330598-overview
- Dahir K, Zanchetta MB, Stanciu I, et al. Diagnosis and management of tumor-induced osteomalacia; perspectives from clinical experience. J Endocr Soc. 2021;5(9):bvab099.
- Kuro-o M. The Klotho proteins in health and disease. Nat Rev Nephrol. 2019;15(1):27–44.
- Napoli N, Conte C. Bone fragility in type 1 diabetes mellitus: new insights and future steps. Lancet Diabetes Endocrinol. 2022;10(7):475–476.
- Sheu A, Greenfield JR, White CP, et al. Assessment and treatment of osteoporosis and fractures in type 2 diabetes. Trends Endocrinol Metab. 2022;33(5):333–344.
- Giacomelli G, Meriggiola MC. Bone health in transgender people: a narrative review. Ther Adv Endocrinol Metab. 2022;13. doi:10.1177/20420188221099346
- Daya NR, Fretz A, Martin SS, et al. Association between subclinical thyroid dysfunction and fracture risk. JAMA Netw Open. 2022;5(11):e2240823.
- Goyal R, Jialal I. Hyperphosphatemia. In: StatPearls. Stat Pearls Publishing, June 2023. https://www.ncbi.nlm.nih.gov/books/NBK551586
- Lewis JL. Hypophosphatemia. Merck Manual. Published Sept. 2021. Updated Sept. 2022. https://www.merckmanuals.com/en-ca/professional/endocrine-and-metabolic-disorders/electrolyte-disorders/hypophosphatemia
Frederick L. Kiechle, MD, PhD
Editor, CAP TODAY Q & A Column
Chief Medical Officer
Boca Biolistics reference laboratory
Pompano Beach, Fla.
Member, CAP Publications Committee
 CAP TODAY Pathology/Laboratory Medicine/Laboratory Management
CAP TODAY Pathology/Laboratory Medicine/Laboratory Management
