Karen Titus
March 2017—The language of blood banking experts, as they talk about irradiators, transfers easily to a car dealership. How reliable are the newer models? Are you willing to replace it every 10 years or so? Do you keep running it until it dies? What parts are likely to burn out? What will repairs run?
And then the word “terrorism” pops up.
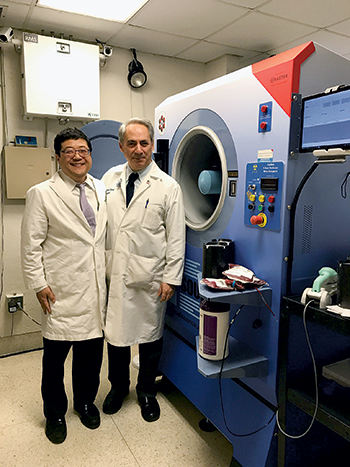
Dr. Jeffrey Jhang (left) and Dr. Jacob Kamen at Mount Sinai Hospital, where the Rad Source RS3400 x-ray irradiator (at right) was installed in January. “We were training, validating, and using the machine in February, and we went live on March 1,” Dr. Jhang says.
Since the Sept. 11 attacks, worries about risks to blood supplies have persisted. Sometimes those fears have burned with intensity; at other times, concern has lingered like a low-grade fever. But they’ve never disappeared. Cesium irradiators have long been used to prevent transfusion-associated graft-versus-host disease as well as in research applications. In the wrong hands, cesium also can be used to make a so-called dirty bomb.
Or worse.
Jeffrey Jhang, MD, associate professor of pathology, Icahn School of Medicine at Mount Sinai, New York City, says he hadn’t given much thought to terrorism scenarios until he spoke about the risks with his institution’s radiation safety officer. He knew about dirty bombs. But other chilling possibilities lurked as well, says Dr. Jhang, who is also director of the blood bank and transfusion services, Mount Sinai Health System.
With ominous visions filling the heads of hospital leaders, it made sense, says Dr. Jhang, to replace Mount Sinai’s cesium irradiators with x-ray irradiators. But as blood bankers at Mount Sinai and other institutions report, doing the “right thing,” as Dr. Jhang puts it, doesn’t mean it’s an easy thing.
For pathologists more used to making decisions based strictly on a cost-benefit analysis, says Dr. Jhang, replacing a cesium irradiator with an x-ray device may not seem like a sensible move. “If you look at my operation, the benefits are not that great,” he says. X-ray irradiators can cost $250,000 to $300,000, with annual service contract costs running $15,000 to $20,000. Moreover, he says, “They are thought historically to have greater downtime, requiring more expensive repairs, and they have heating problems.”
Cesium irradiators, on the other hand, require very little maintenance. “They can be used for many, many years,” Dr. Jhang says, “because the source decays very slowly.” What little maintenance is needed—a rare occurrence, by most accounts—is cheaper.
Advantage, cesium. But factor terrorism into the equation, and perceptions shift.
“I don’t know what the percent risk of it happening is,” Dr. Jhang concedes. “These events are unpredictable. But it could be you.”
That uncertainty led to the decision of Mount Sinai administrators to reduce the risk, despite the cost. “The idea that our hospital could be the center of a dirty bomb attack kept everybody up at night,” he recalls. “So the chief operations officer at our Mount Sinai West facility was very happy to get rid of that cesium irradiator. It would help him sleep at night, help us sleep at night.” The same sentiments coursed through administration at the main hospital, “that if we could do something to reduce our risk, that would definitely be the way to go.”
In fact, says Dr. Jhang, perhaps the hardest person to convince was Dr. Jhang himself.
“I just had to make sure I was comfortable with the notion that a lot of prior problems with x-ray irradiators had been resolved and weren’t going to impact my operations,” he says, noting that older models were known to overheat, “and their x-ray tubes blew frequently, and their power supplies blew frequently.” That meant downtime and unexpected repairs. “That’s something I didn’t want to commit our hospital to, because we are very high volume, and we do rely on irradiating units ourselves, rather than purchasing them.”
Dr. Jhang set his mind at ease by talking to others who had made the switch to newer models. “They seemed much more reliable, with better uptimes and less breakage requiring replacements of key parts, such as tubes and power supplies.”
He cites another advantage: The x-ray irradiator requires less time and labor than the cesium irradiator. While the labor savings aren’t huge, they’re not paltry, either. Dr. Jhang says prior to the replacement, it took about nine minutes to irradiate two units; now, six to eight units can be processed in five minutes.
Mount Sinai’s chief radiation safety and laser officer Jacob Kamen, PhD, CHP, was one of the hospital leaders who saw the advantages of moving radioactive cesium out of the facilities. Mount Sinai recently installed two x-ray irradiators, one for the blood bank and one for research.
Dr. Kamen, who is also senior director of Mount Sinai’s Radiation Safety Department and an associate professor of radiology, recalls the long road to making these changes. While worries spiked after 9/11, simply removing cesium irradiators—as some in the federal government initially demanded—is no quick task.
A renewed push came in 2010, Dr. Kamen says, with the 10-year anniversary of the attacks approaching. Al-Qaeda had been making threats in advance of the anniversary, and administrators were worried about the possible use of radioactive cesium in a dirty bomb to contaminate a large area. “A dirty bomb could cause long-term economic damage,” says Dr. Kamen. Mount Sinai (which at the time had not yet merged with other area hospitals and was simply Mount Sinai Medical Center) seemed like a likely soft target, as did other New York City hospitals, he says.
The first step was to prepare for a worst-case scenario with cesium still in place. The hospital purchased sophisticated equipment to monitor radiation levels, for example, as well as other equipment used by the police department, to make sure both used the same terminology and equipment in an emergency situation, Dr. Kamen says. The hospital set up decontamination facilities and trained security staff how to use them in the event that a large number of contaminated people were to come to the hospital. “We had a lot of drills with the fire and police departments,” he says.
Mount Sinai also collaborated with the federal government, specifically the National Nuclear Security Administration, and the subsection now called the ORS, or Office of Radiological Security. Among other actions, the hospital drastically reduced access to the cesium irradiator used for research. At the time, 144 people used the research device, Dr. Kamen says. It made more sense to have one person perform irradiation tasks for everyone; that person underwent FBI background checks.
Securing the blood bank irradiator was harder, given the need for 24/7 access. More staff needed to undergo FBI background checks. And the machines were “hardened”—security speak for making the cesium irradiators unassailable—with measures such as monitoring systems with multiple alarms. “Mount Sinai was the first hospital in New York City to be connected directly to the police department in case any of these alarms goes off,” Dr. Kamen says.
But the risk, while reduced, had not been removed. Given Mount Sinai’s size and status, it didn’t make sense to keep the cesium irradiators. “And at the 2016 Nuclear Security Summit, radiological risk was the key issue,” Dr. Kamen says, with more than 50 world leaders agreeing the highest threat is nuclear and radiological terrorism. Alternative technology is one way to reduce the threat. “The x-ray irradiators are FDA approved,” Dr. Kamen says, “and there’s no need to worry about liability if a radiological event were to occur.” As an added incentive, the health system’s leaders hoped Mount Sinai would inspire other institutions to remove their cesium irradiators if they hadn’t done so already.
The research group was somewhat difficult to convince, since the irradiation tasks its members perform are diverse. “Some researchers perform whole body irradiation on rodents, others perform targeted irradiation, and some perform irradiation on cells,” Dr. Kamen explains.
In response, Dr. Kamen and his colleagues spoke the blunt language of money, explaining that the federal government currently covers the six figures it costs to decommission a cesium irradiator. If the hospital doesn’t migrate to alternative technology now, and in a few years if the U.S. government doesn’t help, grant and other monies could be at risk.
“The researchers at Mount Sinai have come to the conclusion that they will help any way they can,” he says. A handful of researchers did the necessary comparison studies and were reassured that an x-ray irradiator could perform just as well; ongoing studies have since proved that point with the new machine. “We think we’re getting even better results than we were before,” Dr. Kamen says, noting that the x-ray device has 320 kVp—twice the energy of the old machine.
Federal involvement remains a key factor in the equation, with some administrations assigning a higher priority than others, Dr. Kamen says.
 CAP TODAY Pathology/Laboratory Medicine/Laboratory Management
CAP TODAY Pathology/Laboratory Medicine/Laboratory Management
