Anne Paxton
May 2018—If a seismic shift were to happen in microbiology, the technology behind the Accelerate Pheno system and PhenoTest BC test kit, which won FDA approval last year as a rapid pathogen identification and antimicrobial susceptibility testing (AST) system for blood cultures, could well be the cause.
Like Secretariat, leaving the entire field of other racehorses 31 lengths behind to win the 1973 Belmont Stakes, Accelerate Pheno has won recognition for blazing speed. It handily outstrips the turnaround time of traditional ID and AST for microorganisms causing bloodstream infections. Providing both phenotypic minimal inhibitory concentration (MIC) and categorical AST results from positive blood cultures in seven to eight hours—versus the customary 48 hours—the system from Accelerate Diagnostics is changing how quickly clinicians can provide optimal therapy to patients with bacteremia and sepsis, microbiology laboratories report.
The BC kit simultaneously detects and identifies multiple microbial targets—about 92 percent of the most common bacteria and Candida species in a positive blood culture. Where it pulls ahead is with its unique ability to then immediately perform susceptibility testing on the organisms detected.
“From the moment a patient’s blood is collected to the time we can release an ID with susceptibilities—from vein to the electronic medical record—we can do this in about 24 hours instead of three or four days,” says Eric Rosenbaum, MD, MPH, assistant professor of pathology and medical director of clinical microbiology at the University of Arkansas for Medical Sciences. “That has never been possible before—nothing even close.”

Dr. Humphries
“It really is a paradigm shift in how we manage patients who have bacteria in the blood,” says Romney Humphries, PhD, D(ABMM), MT(ASCP), former section chief of clinical microbiology at UCLA Health System, now chief scientific officer at Accelerate Diagnostics. “The traditional approach is that those patients are ‘rounded on’ by a medical team based on data that comes out day by day. Now we’ll have data that’s coming out hour by hour. And we’ll be much more able to modify and manage treatment in a matter of hours.” Multiple sites are already using the Accelerate Pheno system, and “there are over 100 more that are looking at the system as we speak,” Dr. Humphries says.
Dr. Rosenbaum’s laboratory was one of the first to complete system verification studies, successfully design the interface of the Accelerate system with both the laboratory information system and the institution’s EMR, and fully integrate the system and test into patient care. Since becoming medical director in 2011, Dr. Rosenbaum has been on a quest to modernize his laboratory.
“We started off with a MALDI-TOF mass spectrometer, then a GeneXpert. When we began investigating rapid blood culture ID systems, the Accelerate system had just arrived on the market. It challenged our initial plan to evaluate the well-established and successful FilmArray and Verigene systems. The added ability of the Accelerate system to produce rapid susceptibilities was exciting,” he says, “but it was also very new technology.”
In blood culture diagnostics, FilmArray and Verigene employ molecular methods like PCR or nucleic acid testing for finite pathogen identification, while Accelerate, instead of amplifying DNA, uses fluorescence in situ hybridization probes that also target a finite number of bacteria and yeasts. “All these instruments aim to target the most common organisms that cause sepsis and those are the pathogens to which they direct probes, whether they be primers or, in the case of Accelerate, FISH targets,” Dr. Rosenbaum says. Accelerate is able to detect a panel of 16 pathogens: 14 bacteria and two Candida species.
A 2017 study of the accuracy and workflow of ID/AST using Accelerate Pheno compared its performance with routine standard of care. The authors found, for identification, overall sensitivity of 95.6 percent and specificity of 99.5 percent. For AST, overall essential agreement was 95.1 percent and categorical agreement was 95.5 percent compared with routine methods. There was one very major error and three major errors. Time to identification using Accelerate was decreased by 23.47 hours, and time to AST was reduced by 41.86 hours, with reduction in hands-on time of 25.5 minutes per culture (Charnot-Katsikas A, et al. J Clin Microbiol. 2018;56[1]:e01166-17).
Clinical trials of the Accelerate Pheno showed that if a patient’s positive blood culture is monomicrobial—i.e. has only one target pathogen—the instrument has a 99.6 percent positive predictive value when evaluated in combination with the Gram stain, Dr. Rosenbaum says. However, use of a universal probe along with FISH gives Accelerate the additional ability to indicate the likely presence of off-panel organisms. “So if a blood culture grows something off panel, the Accelerate Pheno should generally be able to tell the user, ‘There’s something in this culture; I just can’t identify it.’ This is the first instrument to offer this valuable feature.”
A logistical advantage of the Accelerate approach is that all reactions and analyses are automated, and microbiology bench experience is not needed to run the test 24 hours a day. It is simple to operate and takes about one minute to set up, Dr. Rosenbaum says. “You aliquot half a cc of the positive blood culture into a sample vial, snap the vial into the cartridge, and insert it into the machine. The Pheno system also frees technologist time that would have been spent processing blood culture identifications and susceptibilities from agar plates.” He estimates that the Accelerate saves at least 30 minutes per specimen.
His laboratory has not stopped using the Gram stain, which is run simultaneously with the Accelerate Pheno. The manufacturer says results are intended to be interpreted in conjunction with Gram stain results. “Once a blood culture bottle goes positive, in about 15 minutes we can say, for example, ‘Gram-positive cocci in clusters’ or ‘Gram-negative bacilli.’ These results are released into the medical record and can begin to direct treatment. Then, to the surprise of our clinicians, within hours they have ID and susceptibility results with MICs.” For many organisms, “we are able to de-escalate antimicrobial therapy after just 24 hours.”
The Accelerate Pheno system has freshly emerged from a favorable multicenter evaluation, with the study authors, in an April 2018 article, describing it as unique and a “first of its kind diagnostic system” (Pancholi P, et al. J Clin Microbiol. 2018;56[4]:e01329-17). Clinical impact studies have not yet been completed, but another new study looks retrospectively at patients with Gram-positive bloodstream infections. The study reports on the system’s performance in Monte Carlo simulations, finding that, “coupled with stewardship personnel (either 24/7 or Monday to Friday)” the new approach “would have allowed unnecessary therapy to be stopped and active/targeted therapy to be started ≥ 24 hours sooner in > 50 percent of patients” (Sofjan AK, et al. Ann Pharmacother. Epub ahead of print March 20, 2018. doi:10.1177/1060028018765486).
Dr. Rosenbaum points to striking case-based evidence that his institution’s clinical use of the system is changing treatment of sepsis for the better. The recent case of a 22-year-old kidney transplant patient presenting with fever, chills, and rigor is illustrative, he says. Clinicians suspected sepsis of unknown etiology, so they prescribed piperacillin/tazobactam (Zosyn) plus vancomycin. “With use of the system, the clinical team knew within 24 hours that the blood cultures collected on presentation were growing a pan-susceptible E. coli, so the team de-escalated to ceftriaxone monotherapy immediately.”
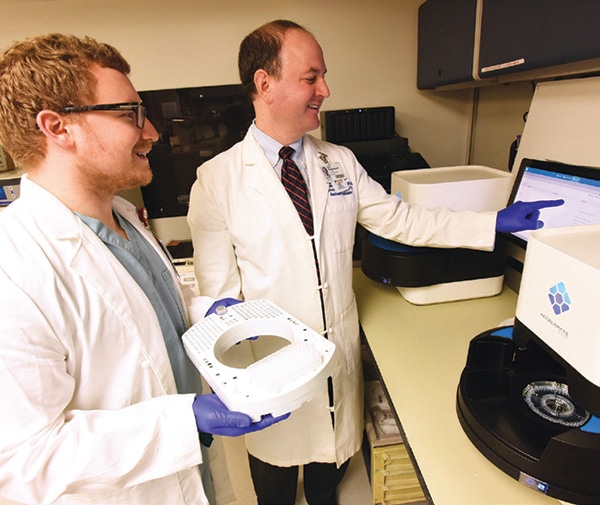
Dr. Eric Rosenbaum (right) and pathology resident Jonathon Gralewski, DO, in the University of Arkansas for Medical Sciences clinical microbiology lab with the Accelerate Pheno. All reactions and analyses are automated, Dr. Rosenbaum says, and bench experience is not needed to run the test 24 hours per day. Photo credit: John Paul Jones, UAMS
This patient was also spared the cumulative risk of acute kidney injury caused by an extra two to three days of broad-spectrum Zosyn and vancomycin—the time it would have taken conventional methods to produce antibiotic susceptibility results. “Nephrotoxity is one of the greatest downsides of using antibiotics like these,” which can significantly increase the odds of acute renal injury, Dr. Rosenbaum notes. Complications of AKI can prolong hospital stays from days to a week or more, even in patients with no preexisting renal compromise.
Dr. Rosenbaum also points to a 64-year-old patient with myeloma and febrile neutropenia who presented to the emergency department, triggering use of a broad-spectrum antimicrobial. “The clinical team started the patient on meropenem, concerned about an infection resistant to something like cefepime.” His laboratory was able to run the sample on the Accelerate Pheno and find out in 24 hours that the organism was, again, a pan-susceptible E. coli. “So the patient could be switched quickly from meropenem to narrower-spectrum cefepime, which is a win for antibiotic stewardship,” Dr. Rosenbaum says.
Getting such a significant head start on appropriate treatment has to be factored in when considering the cost of the test, Dr. Rosenbaum says. “There is a price difference. But the resources we spend on Pheno are captured back exponentially by the prompt clinical action this instrument enables. For example, switching from daptomycin—used against enterococci—to ampicillin is great not only for antibiotic stewardship but also for fiscal accountability. A patient may not need to be on a drug that is 10 times the cost, and we are now able to know this information days earlier.”
Before moving Accelerate Pheno to clinical use, Dr. Rosenbaum says, his laboratory put it through rigorous challenges, some exceeding physiologic conditions required for verification studies. Equally important was surveying how clinicians would react to the dramatic change of receiving ID and AST results finalized within hours. “Before we signed the contract, I gathered clinicians together throughout our hospital who frequently order blood cultures. We talked about what they would do with a call from the laboratory in the middle of the night with an Accelerate Pheno result. It’s very easy to stay the course, but switching the patient to a more appropriate antibiotic as fast as possible is crucial to making the Pheno a success.” Because this is such a major change, there is a learning curve, he notes. The lab must recruit help from the antibiotic stewardship and infectious disease teams to move things along.
With microbiology data, it’s easy for clinical staff from a resident on up to understand when a patient is on the wrong antibiotic for a particular bacterium, says Dr. Humphries, who led the clinical study of Accelerate Pheno at UCLA, one of 13 trial sites. “Conversely, when a patient is being treated unnecessarily broadly, we all appreciate that overtreatment is bad too. But the same urgency isn’t typically placed on de-escalating treatment. So the most effective use of our Accelerate Pheno system in conjunction with the antibiotic stewardship team is to help physicians understand that and help with the de-escalation.”
Molecular testing has improved AST, but it has limitations. “Bacteria are very creative beings,” she notes. “Usually their resistance, especially for Gram-negative blood cultures, is very complex. So it’s very difficult to do a PCR for a single gene and predict antibiotic susceptibility or resistance. Even if we have the entire genome, today we don’t know enough about it to be able to look at all the genes and say, ‘That bacteria is susceptible to the antibiotic I want to use.’” Since genotypic approaches to AST can’t fully predict susceptibility or resistance, if a target is detected, the result must report resistance, Dr. Humphries explained in a presentation at ASM Microbe 2016.
In diagnostics, there’s been a steady progression in the movement toward more rapid identification of bacteria and susceptibility testing, she says. “The big, big difference with our system, compared to others on the market or that are standard of care, is the very, very fast susceptibility testing result, which tells physicians what drug to treat the patient with.”
“Even if the bacteria have mutated and there is brand-new resistance, it doesn’t matter; the system will still detect it. And that’s really the Holy Grail of doing fast susceptibility testing.”
When Beth Prouse, MS, MT(ASCP), clinical microbiologist at Peninsula Regional Medical Center, Salisbury, Md., a freestanding community hospital, first heard about Accelerate Pheno in summer 2016, her laboratory was immersed in building its new Epic Beaker LIS. But soon after the FDA approval of Accelerate, she went for training on the instrument and began the verification process. “We were already using rapid technology for identification of bloodstream infections for a positive blood culture, using the Verigene. We wanted to see what impact getting susceptibility results in such a rapid time frame would have on our patient care and antimicrobial stewardship.”
The morphokinetic analysis that underpins Accelerate’s susceptibility testing involves the instrument taking pictures of the isolate growing in a certain concentration of an antibiotic, Prouse says. “Then the system looks at how the organism either grows or dies off, and compares those photographs to a library.” Dr. Rosenbaum describes this morphokinetic cellular analysis as “an ingenious merger of computer science with medicine.
“About 148 billion data points are analyzed per run,” he says, “generating growth patterns that are compared to an extensive database of known growth behavior correlated to broth microdilution methods in order to produce MICs.”
At Peninsula Regional Medical Center, with susceptibility results available to physicians 48 hours sooner than when they were performed directly on the blood culture bottle, brisker communication between the clinical pharmacists and clinicians is one of the major impacts so far. Says Prouse: “We page our clinical pharmacists several times during the process, letting them know when the patient sample is going on the Accelerate Pheno system, when the ID is done, and when susceptibilities are completed. At that point, they communicate with the clinicians, and antibiotics can be de-escalated. With Verigene, we would let the clinical pharmacists know if there was a resistance marker present, but we didn’t contact them if it wasn’t,” so that communication was primarily related to escalation of antibiotics.
In the emergency department, Peninsula Regional has always had a fairly aggressive approach to identifying patients with sepsis early, Prouse says. “With the introduction of the Verigene in 2013, we’ve tried to provide our clinicians with as much information as we can, as soon as possible. Our administration has been very supportive of finding the best technology to do that.”
At a list price of about $250 per test, the PhenoTest BC kit is probably one of the more expensive technologies on the market right now, she notes. “But there’s really not anything else like it on the market. I think it’s a wonderful technology—that’s why we were an early adopter. We’re not an academic center, we’re not a teaching hospital. We’re a community hospital. But I believe this technology can be done in a lab that has good medical lab scientists working in it. It’s not something you have to have a lot of specialized training to perform. But it’s definitely a team effort to make sure patients are getting better care based on the results.”
Beginning in May, Prouse says, Peninsula plans to conduct a formal six-month study to confirm the clinical outcomes relating to length of stay, mortality, and antibiotic use.
Margie Morgan, PhD, professor of pathology and laboratory medicine and director of microbiology at Cedars-Sinai Health System in Los Angeles, first heard of Accelerate when she was asked to attend a focus group discussion of a new type of technology described as “divergent.” Soon after, Cedars-Sinai became another site for the clinical trial.
Using the system from Accelerate, she says, “we can take an aliquot from the positive blood culture, inoculate the Accelerate Pheno, and within one hour and 20 minutes, be able to alert the clinician to what organism has been identified, and about five and a half to six hours later, report the final susceptibility.”
 CAP TODAY Pathology/Laboratory Medicine/Laboratory Management
CAP TODAY Pathology/Laboratory Medicine/Laboratory Management
