Amy Carpenter Aquino
October 2018—How pregnancy affects normal thyroid function and thyroid function tests, and screening for thyroid disease during pregnancy, were the focus of a session at this year’s AACC annual meeting.
Ann M. Gronowski, PhD, DABCC, a professor of pathology and immunology, and of obstetrics and gynecology, Washington University School of Medicine in St. Louis, opened with an interactive question that addressed how the pregnant state affects normal thyroid function and thyroid function tests. Attendees disagreed on whether thyroid-stimulating hormone increases, decreases, or stays the same during pregnancy.
“You’re in the right place to find out,” Dr. Gronowski said. “The correct answer is that generally it decreases during the first trimester.”
Dr. Gronowski’s co-presenter was Joely A. Straseski, PhD, DABCC, of ARUP Laboratories.
Six main changes occur to the thyroid during pregnancy. The first one Dr. Gronowski addressed is that the high concentration of estrogen changes the thyroxine-binding globulin (TBG) glycosylation, which increases the half-life of the protein. The liver increases TBG production and reduces TBG clearance, which contributes to the two- to threefold increase in the amount of serum TBG concentrations. The TBG concentrations reach a plateau at about mid-gestation and remain elevated. “The affinity of T4 for TBG doesn’t change at all,” Dr. Gronowski said.
Second, as a result of the increase in TBG concentration, “you see a parallel increase in the concentrations of total T4 and total T3” around the 20th week of gestation. “Therefore, we can’t really use the normal reference intervals for total T3 and total T4.” The general practice is to multiply the upper reference level by 1.5 to get pregnancy-specific reference levels for total T3 and total T4.
Third, the protein hCG, which is a member of the pituitary glycoprotein family that has homology with TSH, LH, and FSH, can bind to the TSH receptor and has weak intrinsic thyrotropic activity. “During pregnancy, in the first trimester when hCG concentrations peak around weeks eight to 12, you see slightly decreased concentrations of TSH,” Dr. Gronowski said.
Surprisingly, only about three percent of women have an elevated free T4 concentration as a result. In this “kind of weird, inverse relationship,” she said, TSH decreases while hCG increases. TSH tends to stay within the normal reference interval, though some women may go outside the interval. A study she and colleagues conducted looked retrospectively at 16,000 physician-ordered hCG concentrations and found 69 samples from 63 women in which concentrations of hCG were greater than 200,000 IU/L (Lockwood CM, et al. Thyroid. 2009; 19[8]:863–868). “When you get concentrations above 400,000 IU/L, 100 percent of TSH in those women was below 0.2 mIU/mL. There is clearly this inverse relationship, especially as concentrations get very, very high.”

Dr. Gronowski
An increase in serum thyroglobulin is the fourth change to the thyroid during pregnancy. “Thyroglobulin itself lacks specific hormonal activity. Elevated concentrations can indicate increased thyroid status or injury to the gland. In pregnancy, it indicates an increase in activity.”
Thyroglobulin is produced by the follicular cells and is a precursor of the thyroid hormones. “Due to this increased demand for T4 in the first trimester, it’s associated with an increase in thyroid volume.” As pregnancy progresses, Dr. Gronowski said, “we shift to higher serum concentrations of thyroglobulin.”
An increase in renal iodine clearance is change No. 5. The increase in the glomerular filtration rate causes pregnant women to lose iodine renally, but this is compensated for by an increase in thyroid iodine clearance. This results in an increased dietary requirement for iodine, and in iodine-deficient areas it can result in goiter.
In the United States, where iodine intake is sufficient, the average increase in thyroid size is about 10 percent. In iodine-deficient areas, a size increase of more than 30 percent can be seen. Women in ancient Egypt and ancient Africa were believed to have tied a thin reed around their necks; when the reed broke as a result of goiter, it was an indication of pregnancy.
Change No. 6 is a decrease in serum free T4 concentrations. “You may see slight increases in the first trimester,” Dr. Gronowski said. “hCG concentration is high in its stimulant for thyroid.” The remainder of pregnancy, however, is marked by a decrease in serum free T4 concentrations. “This is due to the increase in TBG concentrations, the increase in renal iodine clearance, and an overall increase in the demand for T4.”A 2007 study illustrated the decrease in free T4 whether measured by tandem mass spectrometry or immunoassay (Kahric-Janicic N, et al. Thyroid. 2007;17[4]:303–311). Despite the clarity of the measurements, “there’s been a lot of debate about this concept over the years,” she said. The question people ask is, “If TSH is normal, shouldn’t free T4 be normal?”
Dr. Gronowski referred to a 2009 study in which 93 nonpregnant patients were compared with 111 pregnant patients (Lee RH, et al. Am J Obstet Gynecol. 2009;200[3]:260.e1–e6). All patients were thyroid peroxidase antibody negative with no predisposition to thyroid disease and were screened using two immunoassay methods (Roche Elecsys and Tosoh A1A-600) to measure urinary iodine total T4 concentrations, TSH, and free T4.
The authors calculated the free T4 index, “a calculated value based on the total T4 concentration in the thyroid binding capacity,” one that provides a measure of the available thyroxin binding sites, Dr. Gronowski explained.
The index is not an estimate of free T4 concentrations, she said. “It’s just assessing if the amount of total T4 that’s there can be accounted for by the amount of binding protein that’s present,” similar to calculations for free versus total calcium.
The free T4 index “was valuable in an era when reliable, commercial free T4 assays were not available,” she added. “But now we have reliable free T4 assays, and we have free T4 by other, more reliable methods”—equilibrium dialysis and mass spectrometry.
The 2009 study examined nonpregnant and first, second, and third trimester TSH measurements, by immunoassay and mass spectrometry. “In the first trimester, TSH dropped slightly because hCG is rising, just as we expected,” she said.
The study’s authors looked at two immunoassay methods for free T4 and found a significant decrease in free T4 concentrations in the second and third trimesters with both methods.
In studying the free T4 index, however, researchers saw a slight increase in the first trimester only. “So they concluded that total T4 and the free T4 index retained an appropriate inverse relationship with TSH throughout pregnancy and appear to provide a more reliable free T4 estimate,” Dr. Gronowski said.
They were in favor of returning to the old method of the free T4 index because it maintains a relationship viewed as more appropriate. However, “they didn’t measure it by equilibrium dialysis, which is really what we consider the gold standard,” Dr. Gronowski said. “I would argue that there are conditions where you have this discordance between TSH and free T4,” she said, comparing it with euthyroid sick syndrome.
As illness progresses, “T3 decreases first, and eventually total T4 and free T4 will decrease as well. TSH generally stays within the normal range, and you’ll see an increase in reverse T3. That’s a natural process—the body is attempting to decrease the amount of T4 that’s converted to T3. I would argue that sick euthyroid syndrome is very similar to late pregnancy.”
In late pregnancy, free T4 and free T3 are low while TSH generally stays within normal limits. “Studies have shown that we see an increase in reverse T3, so it’s actually very similar to sick euthyroid syndrome, which makes physiological sense.”
 The difference between euthyroid sick syndrome and late pregnancy is that in pregnancy there is an increase in total T3 and total T4 because of the increased TBG. In euthyroid sick syndrome, “generally we see a decrease in total T4 and total T3. The difference is in the binding protein. We actually see this in other sick conditions, such as acute hepatitis B.”
The difference between euthyroid sick syndrome and late pregnancy is that in pregnancy there is an increase in total T3 and total T4 because of the increased TBG. In euthyroid sick syndrome, “generally we see a decrease in total T4 and total T3. The difference is in the binding protein. We actually see this in other sick conditions, such as acute hepatitis B.”
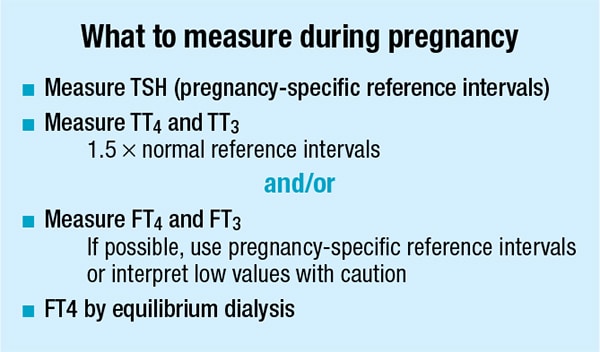
As for what to measure during pregnancy, Dr. Gronowski said, “We can reliably measure TSH. It’s handy if you have pregnancy-specific reference intervals. You can measure total T3 and total T4, adjusting the upper limit by 1.5. You can measure free T4 and free T3, and it’s useful to have pregnancy-specific reference intervals.” Many have been published.
“Our gold standard is always measuring free T4 by equilibrium dialysis. I don’t think we need to go back to free T4 index,” she added.
In an overview of normal fetal physiology, Dr. Gronowski said fetal thyroid follicles develop by 12 weeks of gestation, and by 13 weeks, fetal T4, TBG, and TSH concentrations have increased. T3 does not rise until the third trimester owing to late type I deiodinase production.TSH and thyroglobulin do not cross the placental barrier. Estradiol and hCG are produced by the placenta, so they do cross over to the mother. Early in fetal development, maternal T3 and T4 cross the placenta, but the placenta becomes less permeable as the fetus begins to produce more T4. “It’s important to note, though, that hypothyroidism will still occur in the fetus even when the mother’s thyroid concentrations are normal,” Dr. Gronowski said. “Mom’s thyroid is not enough to compensate for a deficiency in an infant.”
Iodine, some drugs, thyrotropin-releasing hormone, and IgG immunoglobulin can cross the placental barrier.
 CAP TODAY Pathology/Laboratory Medicine/Laboratory Management
CAP TODAY Pathology/Laboratory Medicine/Laboratory Management
