Karen Titus
September 2018—Leo Tolstoy is not listed as a coauthor on the most recent iteration of The Cancer Genome Atlas on renal cell carcinoma, which focuses on molecular characterization of RCC. But the topic is as rich and complex as a Russian novel, and the authors’ approach is so comprehensive, it’s tempting to picture them at least holding forth at a certain soirée in Saint Petersburg (minus the after-party drunkenness and the bit with a bear, of course).
The project may not be as sprawling as War and Peace, which marches 559 characters, speaking two languages, over four volumes, 15 parts, and 333 chapters. It’s a heroic effort nonetheless. There is much to keep track of in renal cell carcinoma, both generally and in this latest document (Ricketts CJ, et al. Cell Rep. 2018;23[1]:313–326.e5), which evaluates 843 RCCs from three major histologic subtypes, including 488 clear cell RCC, 274 papillary RCC, and 81 chromophobe RCC. “And remember,” says actual coauthor Victor Reuter, MD, “this is our fourth publication on kidney cancer.” The previous three each focused solely on one of the subtypes.
The most recent publication expands matters, looking at larger numbers of cases in each category and eyeing them a bit differently, says Dr. Reuter, vice chairman of the Department of Pathology, Memorial Sloan Kettering Cancer Center, and professor of pathology and laboratory medicine, Weill Cornell Medical College. “It’s a natural progression to the other three stories,” he says. “And it shows some novel information as well.” Molecular perspectives—mutations, copy numbers, RNA, microRNA expression studies, methylation, etc.—enabled researchers to look at each group and show differences as well as similarities within each “basket,” he says.
The TCGA, says coauthor Maria Merino, MD, confirms that the spectrum of kidney cancers is indeed quite ample. “And as pathologists, we need to classify these tumors as far as we can.”
Physicians don’t necessarily have to do a deep dive into the paper to realize the implications of its contents. As part of their big data dive, the researchers also looked at patient survival. Moreover, therapies will be targeted to specific tumor types, plain and simple. “If we don’t do this classification and subclassification and confirm them with the genetics, it is possible that patients may not be treated appropriately,” warns Dr. Merino, chief of translational surgical pathology and a principal investigator, National Cancer Institute. This latest installment is yet another chapter in the bigger, ongoing story of how pathologists and others are unmasking the true nature of these tumors.
The work “has been humbling,” says coauthor W. Marston Linehan, MD, chief of the Urologic Oncology Branch, NCI, who has worked on all four TCGA projects. “It’s so complex.”That complexity has been mirrored in clinical practice. “There have been a lot of changes going on in this field in general,” says Donna Hansel, MD, PhD, professor of pathology and chief of anatomic pathology, University of California, San Diego. The biggest, she says, has been the swing toward molecular diagnostics.
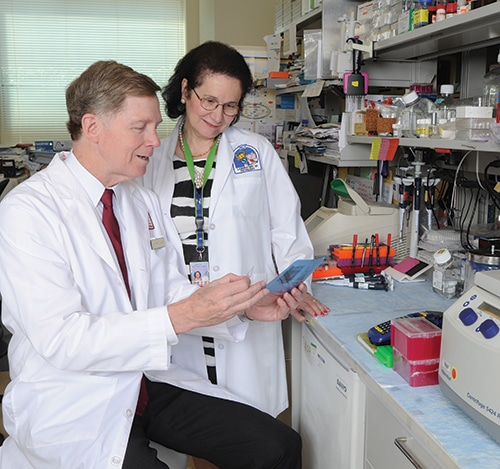
Dr. W. Marston Linehan and Dr. Maria Merino at the National Cancer Institute. “If we don’t do this classification and subclassification [for RCC] and confirm them with the genetics, it is possible that patients may not be treated appropriately,” says Dr. Merino. [Photo: Robert Williams]
Dr. Linehan agrees. “Knowledge is power. And the first step in developing effective forms of therapy is to understand what your targets are.”
Though many of the morphological classifications and subclassifications aren’t necessarily new to pathologists, Dr. Hansel says, the paper highlights some overlapping molecular features of many of them, which haven’t been widely appreciated. That, in turn, has launched countless questions as pathologists try to connect the dots between morphologies and molecular alterations. Are there morphological clues that point to a specific mutation, translocation, or chromosomal abnormality, which would trigger further testing? And if such testing is done, what, if anything, do the results mean?
Dr. Hansel sees a large role for molecular testing. “But how far will that go?” she asks. For her, the most pressing question is whether molecular testing will become the modality for subclassifying tumors. “Or is there still a role for morphology in triaging?” she asks. “I’d like to say there’s a role for both—or else you’re going to get a lot of angry letters,” she tells CAP TODAY.
Perhaps only a fool (fun fact: the chief fool in War and Peace was Napoleon Bonaparte) would argue against any role for molecular, given the changes it has wrought in the field already.

Dr. Hansel
For years, Dr. Hansel says, renal tumors generally were classified into four types of lesions. “And if you didn’t know, you’d just wave your hands and say it was unclassified,” she says, only somewhat jokingly. Over the past 15 years or so, through molecular work primarily but also improved morphology classification, “We’ve gotten much, much better at being able to subdivide these. When you take a look at what we used to call unclassified, a lot of that has shrunk away. We can now put them into very specific baskets.” And new knowledge has upended some baskets entirely.
The “unclassified” basket was “an easy out, in a way,” says Dr. Hansel. It still exists, but only after tumors have been more thoroughly worked up with molecular tools to look for either chromosomal abnormalities or translocation—two of the more common findings in renal cell carcinoma.
Knowing it’s possible to tip some tumors out of the unclassified basket, however, doesn’t mean dropping them in the right basket is a slam dunk. Immunohistochemistry isn’t foolproof. It can lack specificity. Some antibodies have been studied only in small series of tumors; others are quite finicky.
Even when IHC is firing on all cylinders, “The truth is, I continue to see renal tumors that defy classification,” Dr. Hansel says. These cancers exhibit complex and diverse histologies and comprise what Dr. Hansel calls “a maze of tumors, with a whole spectrum of immunohistochemical and molecular changes that accompany them. And trying to put them in the right bucket, and even knowing the bucket exists, has been challenging.”
Complicating matters, renal cell carcinomas seem to be prone to name changes. In some cases, the same tumor is called by different names—not unlike the malleably named characters in The Brothers Karamazov (to borrow from another Russian author).Ever since the new WHO classification came out in 2016, Dr. Hansel says, it has been apparent to her that urologists aren’t always certain of what the changes entail. “So you could be reporting on something they haven’t really heard about before,” she says. They might not know what the classification means; they might also misinterpret what it means.
Dr. Hansel has a simple strategy for this, too: Whenever she makes a diagnosis involving an uncommon category or a new classification, she picks up the phone and calls the clinician. It’s not unusual, she says, for clinicians to hear a word in the name and confuse it with something else (a concept familiar to readers trying to keep up with those Karamazov siblings, all of whom share a middle name—Fyodorovich—and are prone to nicknames as well). There is clear cell renal cell carcinoma, which is not the same as clear cell papillary renal cell carcinoma, which, in turn, is not the same as papillary renal cell carcinoma. “If you have one of those cases, you just want to have a dialogue with the urologists to make sure you’re all on the same page,” Dr. Hansel says.
Dr. Merino concurs. Practicing pathologists (and their clinical colleagues) may not need to absorb every last detail of the molecular analyses presented in the TCGA, “but they should at least see how we classify them,” she says, so they can use the same nomenclature.

Dr. Reuter
Then there are the names that vanished as subclassifications improved. Dr. Reuter alludes to the earlier RCC classifications, when the WHO defined four entities of kidney cancer: clear cell renal cell carcinoma, papillary renal cell carcinoma, granular cell-type renal cell carcinoma, and sarcomatoid renal cell carcinoma.
By the 1990s, pathologists realized neither sarcomatoid carcinoma nor granular cell-type renal cell carcinoma were true entities, and that papillary tumors were rather heterogeneous. By combining good pathology, good IHC, and good molecular biology, Dr. Reuter says, “we were able to tease out a lot of those groups, and understand the morphologic diversity that would be acceptable within each tumor type, as well as its genotype.”
But morphology alone is no longer sufficient to classify a tumor, a point driven home multiple times in the TCGA paper. “If pathologists read it with an open mind, they will see there is a good correlation between pathology and molecular,” Dr. Merino says.
Papillary renal cell carcinoma offers a good example of how matters are evolving. Since the 1990s, says Dr. Reuter, these tumors had been subdivided into Type 1 and Type 2. As it turns out, Type 1s are morphologically indistinct from papillary tumors arising in familial papillary renal cell carcinoma. The hereditary ones, however, characteristically have mutation of MET oncogene present on chromosome 7. (They also are usually diagnosed in patients at a younger age and more likely to be multifocal or bilateral.) Sporadic papillary Type 1 cancers do not have mutations of MET nearly as frequently but are likely to harbor amplifications of the same gene.
Type 2 tumors, Dr. Reuter continues, are morphologically distinct in that they’re more likely to have eosinophilic cytoplasm, high nuclear grade, and prominent nucleoli. But these tumors share an overlapping morphology with other types of tumors, including high-grade Type 1 papillary renal cell carcinomas. Others with overlapping morphology include tumors associated with fumarate hydratase deficiency, as well as those with translocations of either the TFE-3 or TFE-B gene.
(At this point, a wandering mind in search of lighter fare might find itself thinking that RCC classifications mimic the morphing partnerships behind the Great American Songbook. Who wrote what—Rodgers and Hart? Rodgers and Hammerstein? Kern and Hammerstein?)
In simpler terms, says Dr. Reuter, “Type 2 papillary renal carcinoma is a less-than-pure entity. In fact, it’s not an entity.” Given the encompassing nature of this category, “When confronted with this morphology, a pathologist must consider the differential diagnosis.” The answer can help guide therapy, especially for tumors that might qualify for checkpoint inhibitors, for example. And if a familial cancer is implicated, genetic counseling for family members is in order. “These are lethal tumors,” he warns.
The ongoing confusion is understandable—and widespread. “These tumors,” Dr. Reuter says, “comprise a very large percentage of the cases that people like myself and others get in consultation.”
He credits academic pathologists for educating colleagues in the last five to 10 years, spreading the word about modern classifications and molecular correlates “every chance they get.” Nonetheless, he says, that doesn’t obviate the fact that some of these tumors are rare, nor that the many subclassifications can be confusing. “For that reason it’s not unusual for these tumors that are not absolutely the classic examples to be submitted for second opinions by practicing pathologists.”
It can be hard for pathologists, especially in community practice, to keep all these entities straight when the frequency is low, says Michelle Hirsch, MD, PhD, associate professor of pathology, Harvard Medical School, and chief of the Genitourinary Pathology Division and staff pathologist in the Women’s and Perinatal Division at Brigham and Women’s Hospital. There are at least 10 rare renal tumor subtypes that account for only a few percent of all cases. “You’re talking less than one percent for each of these tumor subtypes. So if you’re in a small practice where you’re not seeing a nephrectomy that often, then you’re definitely unlikely to see these unusual subtypes.” (Although none of these are as rare as Aline Kuragina, who apparently shows up only once in War and Peace, and whose husband, naturally, spells his surname Kuragin.)
Dr. Hirsch’s advice: Stay caught up with reading and attend CME conferences. “At least if you’ve heard about or seen these less common tumors in a lecture, you can seek help from somebody who sees these tumors more frequently or in greater volume.”
Picking up the phone can also be helpful. “If I’m really struggling with a tumor,” says Dr. Hansel, “I call the urologists to get a sense of either their impression of the radiology or how the surgery was—was it difficult to get out? I’m very honest about what I’m struggling with. I feel that sort of communication across the board is very helpful.”
These discussions can help Dr. Hansel decide what comes next. “If you get an indeterminate stain, you debate whether you need to take the extra steps to further classify, understanding that that classification may or may not make a difference,” she says. Is the added TAT worth it? Is the clinician a little worried, or a lot? “Usually those are the cases I’ll call the clinician on. They may know something I don’t. Or, it may not change their management. That’s something a lot of people struggle with.”
Though RCC classifications/sub-classifications can seem at times to be swaying at the rim of a rabbit hole, they are pertinent to patients.Dr. Hirsch says her clinical colleagues at Dana-Farber Cancer Institute are keen to know the subtypes, “particularly in the metastatic setting,” in part because they can determine which clinical trials—some of which they’re designing—might help their patients.
Adds Dr. Merino: “Keep in mind, new protocols open all the time.”
In some cases, tumors once thought to be aggressive may actually be indolent. In other cases, tumors that have been considered more common in one patient population might occur in other groups more frequently.
 CAP TODAY Pathology/Laboratory Medicine/Laboratory Management
CAP TODAY Pathology/Laboratory Medicine/Laboratory Management
