Anne Ford
April 2018—In analyzing cervical tissue, adjunctive use of p16 IHC with H&E-stained slides improves accuracy and sensitivity, according to the results of the Cervical Tissue Adjunctive Analysis study presented by Thomas C. Wright Jr., MD, in a webinar hosted by CAP TODAY and made possible by an educational grant from Roche Diagnostics.
Dr. Wright, professor emeritus of pathology and cell biology at Columbia University, said p16 staining in the study, known as the CERTAIN study, improved pathologist correlation with a panel of expert diagnoses. “It’s something which, in my opinion, is dramatically changing our ability as pathologists to make the correct diagnosis,” he said.
P16 is a cyclin-dependent kinase inhibitor that is involved in the normal cell cycle. “Under normal conditions, when we get release of E2F from the retinoblastoma gene product, the result is cell cycle progression,” he said. “This also gives us very low-level expression of p16 within the cervical epithelium, low enough expression that you cannot see it with routine immunohistochemistry.”
That overexpression of p16 results in a feedback rebinding of E2F to the retinoblastoma gene product, leading back into cell cycle arrest. “So p16 plays a critical role in the normal cell cycle,” he said. “This allows us to cycle between progression and proliferation and cell cycle arrest. In contrast to the normal cell cycle, when we have a transforming HPV infection or oncogenesis of the cervical epithelium, what we know is that E2F is permanently released from the retinoblastoma gene product by binding of the E7 protein of a high-risk HPV. This leads to cell cycle proliferation. We end up with overexpression of p16. We get genetic instability. And the amount of p16, which is expressed now in the deregulated epithelium, is enough that you can identify it by routine immunohistochemistry.”
For more than a decade, studies have demonstrated the clinical utility of staining cervical epithelium with p16, with a strong correlation between p16 staining and a consensus histology diagnosis of HSIL (CIN 2, 3). It’s only more recently that p16 staining has been shown to improve the reproducibility rate of cervical disease diagnosis. “And when we talk about p16 immunostaining, it’s important that we recognize that it’s just not any staining of the epithelium,” Dr. Wright cautioned. “It is a very specific pattern of staining of the epithelium, which is associated with the presence of a CIN 2, 3 lesion. What we want to see is diffuse strong, what we call block positive, staining of both the basal and parabasal cells in the epithelium. . . . We want to see one-third of the epithelial thickness stained by p16 in order to call it positive staining.”
So how strong is this association? Dr. Wright pointed to a 2010 study in which 1,500 adjudicated cervical biopsies were stained with p16 (Galgano MT, et al. Am J Surg Pathol. 2010;34[8]:1077–1087). Ninety-nine percent of the adjudicated CIN 3 diagnoses stained with p16. For CIN 2 lesions, it was 77 percent. Thirty-nine percent of CIN 1 lesions were p16 positive. Only five percent of normal biopsies were p16 positive. “Clearly what this says is that if you’re positive, you’re unlikely to be a normal biopsy. And if you’re CIN 3, almost inevitably you’re going to be p16 positive. And finally—I can’t stress this enough—39 percent of the CIN 1 lesions were p16 positive. So if something looks like a CIN 1, you call it a CIN 1, even if it’s p16 positive.”
In problematic cases and in occult lesions, p16 also plays an important role. Dr. Wright shared an image of a biopsy that at least three pathologists who specialize in gynecologic pathology had called non-CIN in the ATHENA study. “When we do the p16 staining, though, what you can see is there’s a little area of p16 positivity. When you look at higher power at that area with p16 positivity, there’s a substantial amount of cellular atypia present. And this was a very small high-grade lesion which was missed by three pathologists.” He displayed two more cases in which small fragments of high-grade disease were initially missed, then detected once p16 staining was performed. (See “Detection of occult lesions.”)
The objectives of the CERTAIN study were to: 1) evaluate the performance of p16 immunohistochemistry as an adjunctive diagnostic aid to H&E-stained slides for the identification of high-grade disease (CIN 2+ status), and 2) assess the performance of published criteria for selecting which biopsies should be stained with p16.
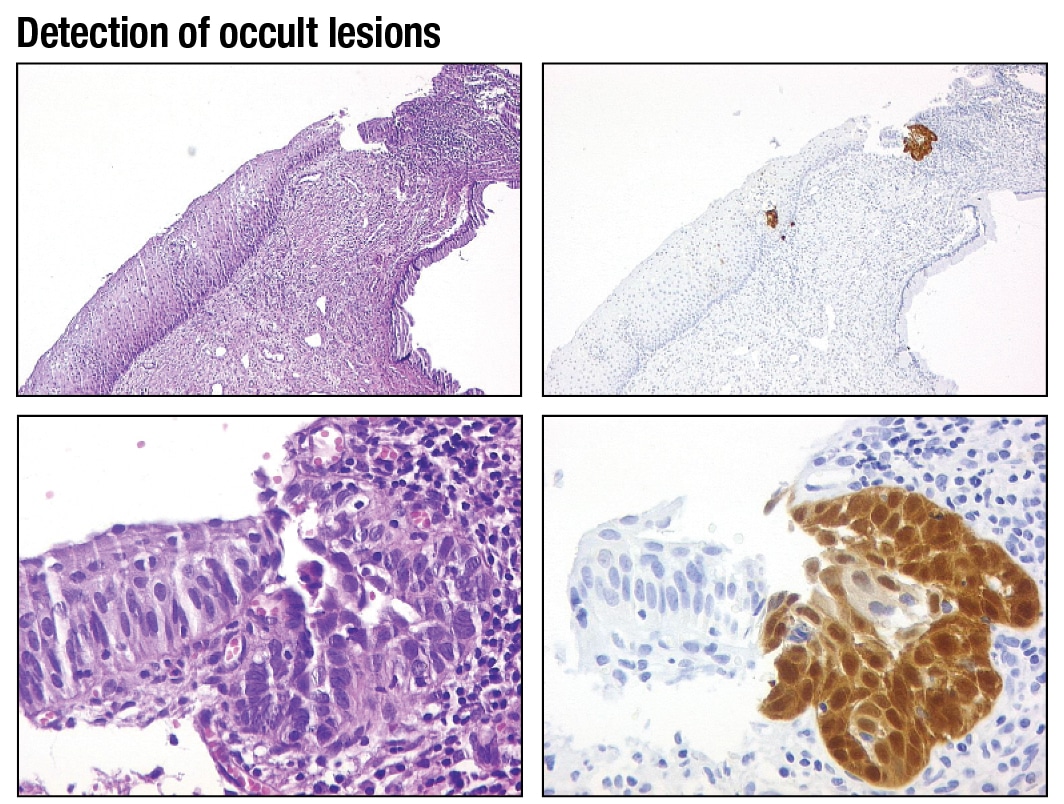
This biopsy was reviewed by three gynecological pathologists and none made a diagnosis of CIN 2, 3. However, p16 staining highlighted a small area of p16 positivity that on high magnification shows considerable atypia. The final diagnosis was CIN 2, 3.
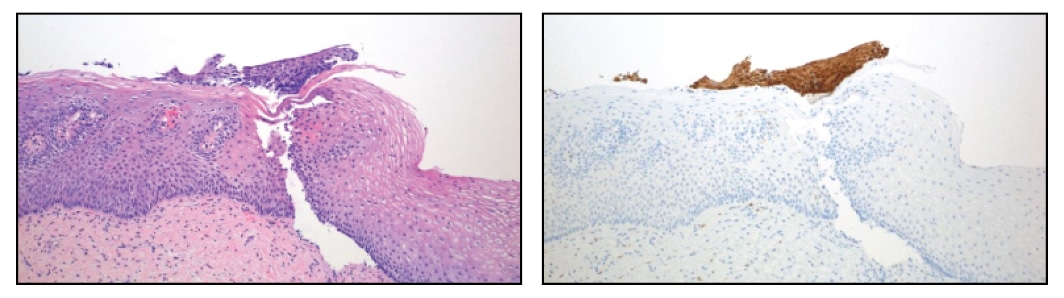
This biopsy has a small detached fragment of atypical squamous epithelium that was either originally overlooked or considered too small to be diagnostic for CIN 2, 3. After p16 staining the case was reclassified to CIN 2, 3 because the detached atypical fragment has strong, diffuse block staining.
 CAP TODAY Pathology/Laboratory Medicine/Laboratory Management
CAP TODAY Pathology/Laboratory Medicine/Laboratory Management
